Deep Vein Thrombosis and Treatment: What to Know
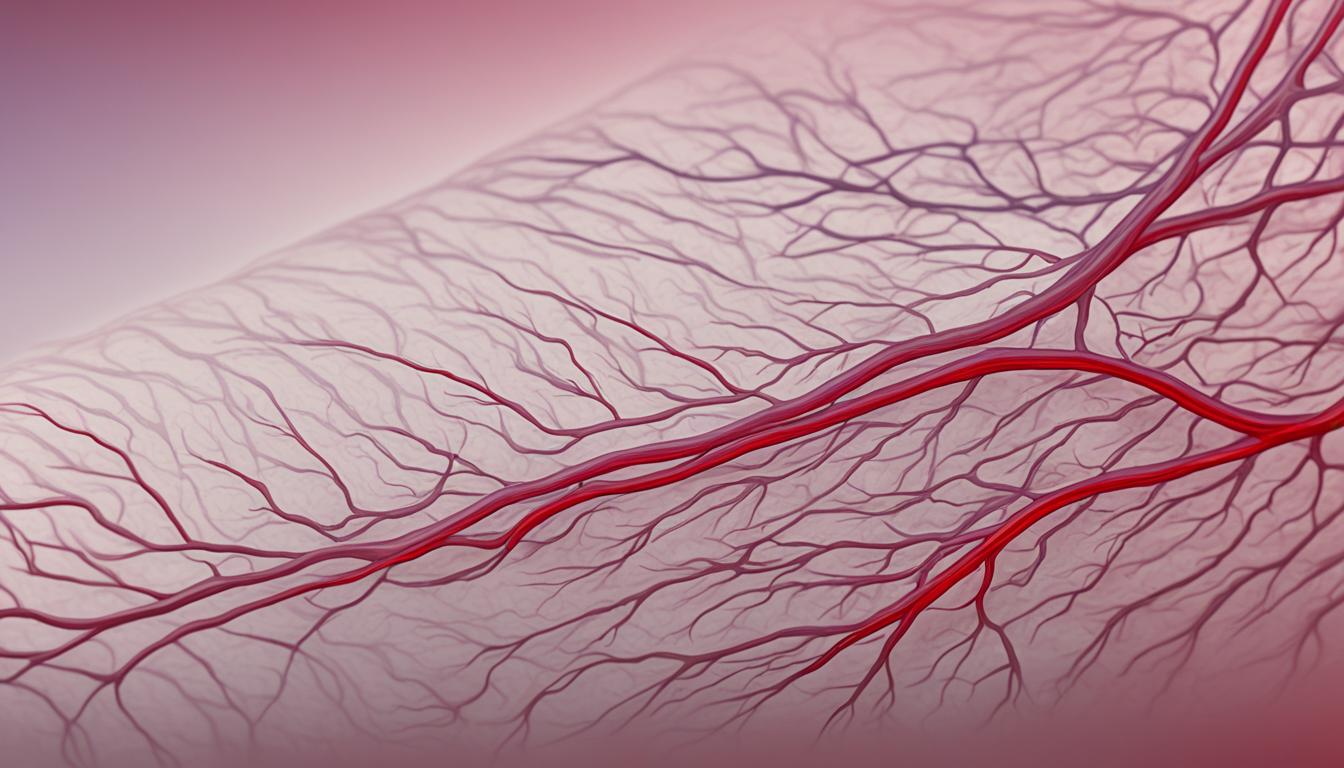
Ever thought if you might get deep vein thrombosis (DVT)? This condition happens when a blood clot forms deep in a vein, usually in the leg. If not treated, it can be very dangerous. It’s important to know about the causes, signs, and ways to treat DVT to keep your blood vessels healthy.
DVT can happen to anyone, but it’s more common in people over 60. Being immobile, injured, having surgery, pregnant, on certain medicines, or having health issues can increase your risk. If you notice your leg hurts, swells, or looks different, you should see a doctor right away.
Key Takeaways
- Deep vein thrombosis (DVT) is a serious condition where a blood clot forms in a deep vein, often in the leg.
- Risk factors for DVT include age, immobility, injury, surgery, pregnancy, certain medications, and underlying medical conditions.
- Symptoms of DVT may include leg pain, swelling, and skin discoloration, and require prompt medical attention.
- Effective treatment options for DVT include blood-thinning medications, clot-busting therapies, and compression stockings.
- Preventive measures, such as staying active, maintaining a healthy weight, and avoiding prolonged sitting, can help reduce the risk of developing DVT.
Understanding Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is a serious condition. It happens when a blood clot forms in a deep vein, often in the leg. This clot is called a venous thromboembolism (VTE). If the clot blocks the blood flow, it can be very dangerous.
If the clot moves to the lungs, it can cause a pulmonary embolism. This is a life-threatening condition.
What is Deep Vein Thrombosis?
Deep vein thrombosis happens when a blood clot forms in a deep vein. These veins are usually in the leg, thigh, or pelvis. The clot can form if the vein gets damaged or if blood flow is slowed down.
This condition is serious and needs quick medical help. It can lead to serious complications if not treated.
Causes and Risk Factors of DVT
Many things can make you more likely to get deep vein thrombosis. These include:
- Age: Getting older increases your risk, especially after 60.
- Immobility: Sitting or lying still for a long time can raise your risk. This includes being bedridden, on a long flight, or after surgery.
- Recent surgery or injury: Injuries to the veins can cause blood clots.
- Pregnancy: Hormonal changes and more blood during pregnancy can increase your risk.
- Certain medical conditions: Some health issues like cancer, heart disease, and inflammatory bowel disease can make you more likely to get DVT.
- Inherited blood clotting disorders: Some people’s genes make their blood more likely to clot.
Knowing what causes DVT helps with prevention and catching it early. This is key to avoiding serious problems.
Symptoms of Deep Vein Thrombosis
Deep vein thrombosis (DVT) can cause various symptoms, but some people might not notice any. The most common signs of DVT include:
- Leg swelling – One of your legs may swell, usually in the calf or thigh.
- Leg pain or cramping – You might feel a dull ache, pain, or cramping in the affected leg. This pain often gets worse when you move.
- Skin color changes – The skin on your leg may look reddish or discolored.
- Warmth in the leg – The affected leg may feel warmer than the other leg.
If you notice any signs of DVT, see a doctor right away. DVT can lead to serious problems like pulmonary embolism, where a blood clot goes to the lungs. Some people with DVT might not have any symptoms. So, knowing the risk factors and getting checked is key.
Knowing the symptoms of DVT and getting treatment quickly can prevent serious issues. If you see any of these signs, don’t wait to talk to a healthcare professional. They can give you the right diagnosis and treatment.
Diagnosis of Deep Vein Thrombosis
Diagnosing deep vein thrombosis (DVT) starts with a physical exam and one or more tests. Your healthcare provider orders these tests to check for a blood clot. They aim to confirm the clot’s presence, location, and how severe it is.
Tests Used to Diagnose DVT
Your doctor might suggest one or more tests to diagnose DVT:
- D-dimer test: This blood test looks for a protein that forms when a blood clot breaks down. A high D-dimer level might show there’s a clot, but it doesn’t pinpoint where it is.
- Duplex ultrasound: This test uses sound waves to see blood flow and spot clots in veins. It’s the main way to diagnose DVT.
- Venography: This X-ray test injects dye into veins to show blood flow. But, it’s not often used today because it’s invasive.
- Magnetic Resonance Imaging (MRI): An MRI scan can help diagnose DVT in the abdomen if other tests don’t give clear results.
The tests your doctor picks will depend on your risk factors, symptoms, and where they think the DVT might be.
“Almost all people with severe Deep Vein Thrombosis (DVT) have increased blood levels of D-dimer protein.”
Getting an accurate DVT diagnosis is key. It lets doctors start treatment quickly to stop serious problems like pulmonary embolism.
Treatment Options for Deep Vein Thrombosis
If you have deep vein thrombosis (DVT), your doctor will help pick the best treatment for you. The main goals are to stop the clot from getting bigger, prevent it from moving to the lungs, and lower the chance of more clots. Here are some common treatments for DVT:
Blood Thinners (Anticoagulants)
Blood thinners, or anticoagulants, are often used to treat DVT. They stop the clot from growing and help prevent new clots. Doctors might prescribe heparin, warfarin, or direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and edoxaban.
Clot Busters (Thrombolytics)
For serious DVT cases, doctors might use clot-busting drugs called thrombolytics. These drugs help dissolve the clot faster than blood thinners. Thrombolytics are mainly for life-threatening clots or high-risk situations.
Compression Stockings
Compression stockings are also part of DVT treatment. They apply pressure to your legs to improve blood flow and reduce swelling. These stockings might be used with other treatments.
The treatment for DVT varies based on your situation and risk factors. It’s crucial to take all medications as directed and keep up with your doctor’s appointments. With the right treatment, most people with DVT can recover and avoid future clots.
“The key to successfully treating deep vein thrombosis is to prevent the clot from growing larger and stop it from breaking off and traveling to the lungs.”
Preventing Deep Vein Thrombosis
Some lifestyle changes can lower your risk of deep vein thrombosis (DVT). This is a serious blood clot that forms in deep veins, often in the leg. By making these changes, you can reduce your risk of a clot that could be life-threatening.
Lifestyle Changes to Reduce DVT Risk
Being active and not sitting or lying down for too long is key to preventing DVT. This means taking breaks during long flights or car rides and doing calf exercises to keep blood flowing. Also, quitting smoking and keeping a healthy weight are crucial. Smoking and being overweight increase your risk of DVT.
- Engage in regular physical activity to promote healthy blood flow
- Avoid prolonged periods of sitting or lying down, such as during long trips
- Quit smoking and avoid tobacco products
- Maintain a healthy body weight through a balanced diet and exercise
By following these lifestyle changes, you can greatly lower your risk of deep vein thrombosis. This condition can lead to serious complications.
“Staying active and maintaining a healthy weight are key to reducing your risk of deep vein thrombosis. Even simple exercises during long trips can make a big difference.”
| Preventive Measure | Benefits |
|---|---|
| Regular physical activity | Improves blood flow and circulation, reducing the risk of clot formation |
| Avoiding prolonged inactivity | Prevents blood stagnation and minimizes the likelihood of clots developing |
| Quitting smoking | Lowers inflammation and improves overall cardiovascular health, decreasing DVT risk |
| Maintaining a healthy weight | Reduces pressure on leg veins and improves blood flow, lowering the chance of clot formation |
By making these lifestyle changes, you can play a big part in preventing deep vein thrombosis. This helps protect your long-term health.
Complications of Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a serious condition that can lead to life-threatening complications if left untreated. The most dangerous complication is a pulmonary embolism, which occurs when a blood clot breaks free and travels to the lungs, blocking blood flow. This can be life-threatening and requires immediate medical attention.
Another potential complication of DVT is post-thrombotic syndrome. This can cause long-term leg pain, swelling, and skin changes due to damage to the veins. Studies show that up to half of people with DVT may develop this syndrome, leading to chronic discomfort and disability.
Prompt diagnosis and treatment of DVT are crucial to prevent these serious complications. Regular medical check-ups and following your healthcare provider’s recommendations can help reduce your risk of developing DVT complications.
Risks and Symptoms of Complications
- Around 1 in 10 people with deep vein thrombosis are at risk of developing a pulmonary embolism (PE).
- Post-thrombotic syndrome affects up to half of people with DVT, leading to long-term effects such as pain, swelling, darkened skin color, skin sores, and varicose veins where the clot was located.
- Pulmonary embolism can cause shortness of breath, sudden chest pain, coughing, and coughing up blood.
- Post-thrombotic syndrome symptoms include pain, swelling, discoloration, and skin changes in the affected leg.
Seeking prompt medical attention and following your doctor’s treatment plan are essential to prevent these serious complications and maintain your overall health. Early intervention can help reduce the long-term impact of DVT.
Deep vein thrombosis and deep vein thrombosis treatment
Deep vein thrombosis (DVT) is a serious condition that needs quick action to prevent serious problems. The main aim of treatment is to stop the blood clot from getting bigger and to stop new clots from forming.
For DVT, doctors often use anticoagulant medications, or blood thinners. These include heparin, warfarin, or newer DOACs. They help stop the clot from growing and prevent new clots. Usually, you’ll take these medications for at least 3 months, based on your risk factors and the DVT’s severity.
Sometimes, more intense treatment is needed, like clot-busting drugs called thrombolytics. These drugs dissolve the blood clot. They are used for severe DVTs or those at high risk of causing a pulmonary embolism.
If you can’t take blood thinners, a vena cava filter might be an option. This small device is placed in the vena cava. It catches any clots that break free and stops them from going to the lungs.
Compression stockings are also often suggested for DVT patients. These stockings apply pressure to the leg. This helps improve blood flow and reduce swelling.
Getting the right treatment for DVT is key because it can lead to serious issues if ignored. By working with their healthcare providers, people with DVT can get the right care. This helps manage their condition and lowers the risk of future blood clots.
Activity Guidelines for DVT Patients
After getting diagnosed with deep vein thrombosis (DVT), it’s key to follow your doctor’s advice on moving and exercising. This means doing calf exercises to help blood flow better, wearing compression stockings, and taking breaks to walk. It’s also important to avoid activities that could cause serious injuries.
Research shows that exercise can make DVT symptoms like swelling and pain better. It helps improve blood circulation and relieves symptoms of venous insufficiency. Activities like walking, hiking, swimming, dancing, and jogging are good for DVT patients. These exercises help push blood up, lowering the chance of blood clots.
It’s suggested to start with short walks of 5 minutes and increase the time as you get stronger. Walking for 5 minutes every hour when sitting for a long time can also help prevent DVT from coming back. Exercises like ankle pumps, leg extensions, and seated marches are also good for DVT patients.
| Exercise | Benefits for DVT Patients |
|---|---|
| Walking | Improves circulation and reduces DVT risk |
| Calf Exercises | Strengthens leg muscles to push blood upward |
| Ankle Pumps | Promotes blood flow and prevents clot formation |
| Leg Extensions | Strengthens leg muscles and improves circulation |
| Seated Marches | Activates leg muscles during periods of prolonged sitting |
By sticking to these activity guidelines, DVT patients can lower the risk of complications and aid in their recovery. Always talk to your healthcare provider for advice tailored to your specific situation and recovery progress.
Self-Care for DVT Management
Managing deep vein thrombosis (DVT) well is key. This means taking your blood thinners exactly as told. You might also need to change your diet because some foods can affect blood thinners. Always watch for signs of too much bleeding, a common side effect of these medicines. If you see any, call your healthcare provider right away. Taking charge of your health helps ensure the best outcome.
Here are some tips for managing your DVT:
- Medication adherence: Always take your blood-thinning medicines as told. Make sure to have regular prothrombin time tests (PT) to check the international normalized ratio (INR).
- Diet changes: Some foods, like leafy greens, can affect blood thinners. Work with your healthcare provider to change your diet if needed to avoid problems.
- Bleeding prevention: Be careful with sharp objects and use an electric razor to avoid cuts that could cause too much bleeding. Call your doctor right away if you see signs of bleeding that’s not normal, like coughing or vomiting blood.
- Lifestyle adjustments: Quit smoking, keep a healthy weight, and exercise regularly to help your recovery and prevent more DVT episodes.
By focusing on self-care and working with your healthcare team, you can manage your DVT well. This reduces the risk of complications.
Your commitment to self-care is vital for handling deep vein thrombosis well. Stay alert, stick to your treatment plan, and ask your healthcare provider if you have any questions or concerns.
Preparing for Your Doctor’s Appointment
If you think you might have deep vein thrombosis (DVT), getting ready for your doctor’s visit is key. Being prepared can help make sure you get the right diagnosis and treatment. Here are some steps to follow before you go:
- Symptom Tracking: Write down all your symptoms, like when they started and what makes them better or worse. This helps your doctor understand what you’re going through.
- Medical History: Collect info about your health history, like any recent illnesses, surgeries, or trips. Tell your doctor about any blood-clotting issues in your family too. This info is important for your DVT risk.
- Medication List: Make a list of all the medicines, vitamins, and supplements you’re taking. This helps your doctor see if any of them might be causing your symptoms.
Having this info ready means your doctor can see your whole health picture. This helps them make a correct diagnosis and plan the best treatment for you. Being well-prepared makes your doctor’s visit more effective.
“The key to a successful doctor’s appointment is to come prepared with all the necessary information. This allows your healthcare provider to make informed decisions about your care.” – Dr. Emily Jamison, Vascular Surgeon
When to Seek Emergency Care
Deep vein thrombosis (DVT) is a serious condition that needs quick action to prevent serious problems. If you have symptoms of a pulmonary embolism, get help right away. Look out for sudden shortness of breath, chest pain that gets worse with deep breaths, a fast heartbeat, feeling dizzy, and coughing up blood.
These signs mean a blood clot has moved to the lungs, which is very dangerous. If you notice any of these symptoms, call 911 or go to the emergency room fast. It’s key to get emergency care for DVT and treat symptoms of pulmonary embolism to stay healthy.
Some things can make you more likely to get a deep vein blood clot. These include major surgery in the leg, hip, pelvis, or belly, being very inactive for a long time, and taking certain medicines like birth control or hormone therapy. Being pregnant or older than 40 also raises your risk.
If you can’t reach your doctor, go to the emergency room if you’re having bad symptoms. They might do tests like ultrasounds, blood tests, and CT scans to check for blood clots in the lungs.
After seeing the ER for DVT or pulmonary embolism, follow up with your doctor soon. You might see specialists like a family doctor, cardiologist, or vascular medicine specialist for more care and advice.
“Seeking emergency care for deep vein thrombosis and addressing the symptoms of pulmonary embolism is crucial for your health and well-being.”
| Symptom | Description |
|---|---|
| Sudden Shortness of Breath | Difficulty breathing that comes on suddenly and unexpectedly. |
| Chest Pain | Pain in the chest that worsens with deep breathing or coughing. |
| Rapid Pulse | A heartbeat that is faster than normal, often over 100 beats per minute. |
| Lightheadedness | Feeling dizzy, faint, or unsteady on your feet. |
| Coughing up Blood | Expelling blood or blood-tinged mucus when coughing. |
Recovering from Deep Vein Thrombosis
Returning to Normal Activities
Getting better from a deep vein thrombosis (DVT) takes time. With the right treatment and care, you can get back to your usual activities. Wearing compression stockings is key to improving blood flow and reducing swelling in the affected leg.
Slowly start doing more physical activities like walking and calf exercises. But, it’s important to listen to your doctor about what activities to avoid. This helps prevent injuries while you’re still at risk for complications.
Most people get better from a DVT in a few weeks or months. The cause of the clot and any other health issues can affect your risk of getting another clot. People with cancer, paralysis, or a family history of blood clots might be more likely to have another clot.
With patience and following your treatment plan, you can manage your DVT and improve your life. Regular check-ups with your doctor will help you recover smoothly and successfully.
“Recovering from a deep vein thrombosis can be a challenging process, but with the right support and care, you can often return to your normal activities and regain your quality of life.”
Long-Term Outlook for DVT Patients
The long-term outlook for deep vein thrombosis (DVT) patients varies. Many recover fully, but there’s a risk of it happening again. This is more likely if the first clot was uncaused or if risk factors are still there.
Post-thrombotic syndrome (PTS) is a big worry for DVT patients. It happens in up to 50% of cases and causes ongoing pain, swelling, and other issues. Damage to the veins is the main cause. Treatment and lifestyle changes can lower the risk of PTS, but it’s still a big concern.
Studies show one-third of people with a DVT will have another clot within 10 years. The risk goes up if the first clot was uncaused, if you have certain health issues like cancer, or if you’re not active or overweight.
To get a better long-term outcome, DVT patients must stick to their treatment plans. This might include blood thinners, compression stockings, and regular doctor visits. Living a healthy life, like keeping a healthy weight, staying active, and not sitting too long, can also help prevent more clots and complications.
“Regular follow-up with a healthcare provider, adherence to treatment, and lifestyle modifications can help minimize the risk of recurrence and long-term complications for DVT patients.”
By knowing the long-term challenges and taking steps to manage their condition, DVT patients can have a better future. They can avoid the bad effects of more clots or PTS.
Conclusion
Deep vein thrombosis (DVT) is a serious condition that needs quick action and the right treatment. It can lead to life-threatening issues like pulmonary embolism. Knowing the signs, risks, and treatment options helps you protect your blood vessels and improve your health.
Studies have shown the effects of DVT on people, especially those at high risk like pregnant women, surgery patients, and those with certain health issues. These findings stress the importance of this condition and its impact on these groups.
If you’re at risk or have DVT, getting medical help is key. Follow your doctor’s advice on treatment and prevention. Making healthy lifestyle changes, taking your medicines, and seeking quick care for symptoms can help manage DVT and lower the risk of serious problems. Your blood vessel health is crucial, and tackling DVT is essential for its protection.
